Executive Summary
Defining the design challenge through stakeholder alignment and outcome mapping
PROBLEM STATEMENT
Market Context & Opportunity
Competitive Landscape: Existing healthtech solutions focused on digitization rather than user experience optimization
Patient Behavioral Shift: Post-pandemic demand for contactless, transparent healthcare interactions
Provider Pain Point: 40% administrative overhead from inefficient scheduling systems
Technology Gap: Limited intelligent queueing systems in regional healthcare markets
Success Metrics Framework
Primary KPI: ≥70% reduction in perceived wait frustration (measured via exit surveys)
Usability Benchmarks: 95% task completion rate, <5% error rate
Business Metrics: 4.5+ app store rating, 80% monthly retention
Operational Impact: 50% reduction in call center appointment requests
Design Objectives
Patient Empowerment: Transform passive waiting into informed, controlled experience
Cognitive Load Reduction: Apply progressive disclosure and smart defaults
Trust Building: Radical transparency in provider information and queue status
Inclusive Design: Cross-generational usability with accessibility-first approach
PRODUCT VISION: After six years of designing consumer and enterprise experiences, I've learned that healthcare UX requires a fundamentally different approach—one that acknowledges emotional vulnerability and time sensitivity. Practo emerged from this understanding: a patient-first platform that transforms the traditionally opaque healthcare journey into a transparent, controllable experience. By applying service design principles and behavioral psychology insights, we created a system that doesn't just digitize appointments—it reimagines the entire care continuum from discovery to follow-up.
DESIGN MISSION: Replace healthcare anxiety with healthcare confidence through intelligent design that anticipates needs, reduces cognitive load, and puts patients back in control of their care journey.
Understanding patient needs through ethnographic observation and behavioral analysis
RESEARCH METHODOLOGY
My research approach combined quantitative behavioral data with qualitative emotional insights. Having spent years observing how users interact with high-stress digital environments, I knew that traditional usability testing wouldn't capture the full picture of healthcare anxiety. Instead, I employed a mixed-methods approach that included contextual inquiries in actual waiting rooms—watching how people naturally behave when they're worried about their health and pressed for time.
TARGET USER SEGMENTATION
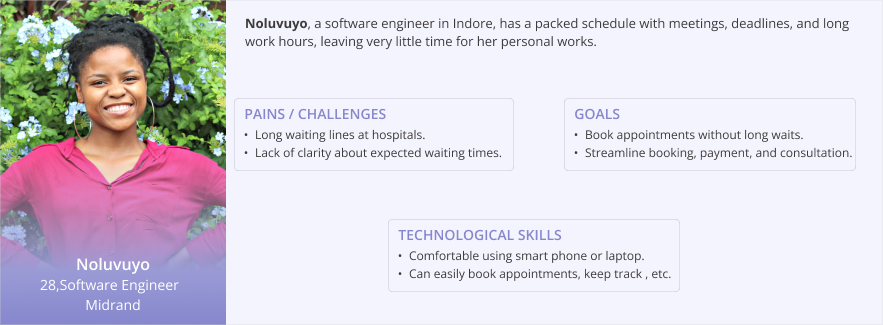
Through demographic analysis and behavioral clustering, two primary personas emerged that represented 85% of our user base:
Behavioral Drivers: Time scarcity, efficiency-focused, comfort with technology
Pain Points: Inflexible scheduling, lack of provider transparency, inefficient communication
Goals: Minimize time investment, maximize appointment value, seamless digital experience
Context: Often booking during work hours, need mobile-first solutions
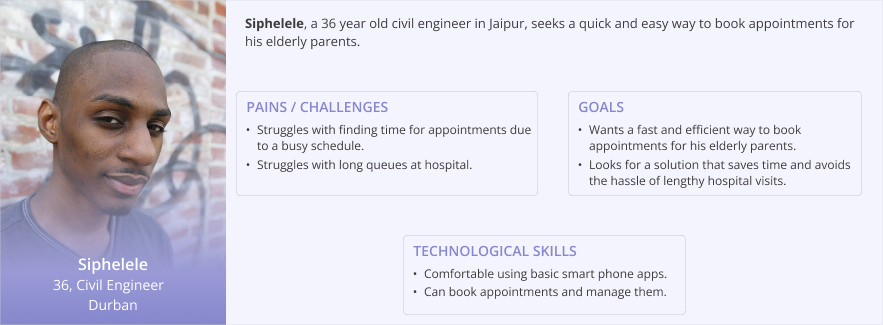
Behavioral Drivers: Managing multiple family health needs, preference for human connection
Pain Points: Complex booking for others, unclear provider credentials, appointment coordination
Goals: Trusted provider selection, clear communication, simplified proxy booking
Context: Managing elderly parents or children, need for delegation features
USER PERSONAS
PRIMARY RESEARCH: EMOTIONAL JOURNEY MAPPING
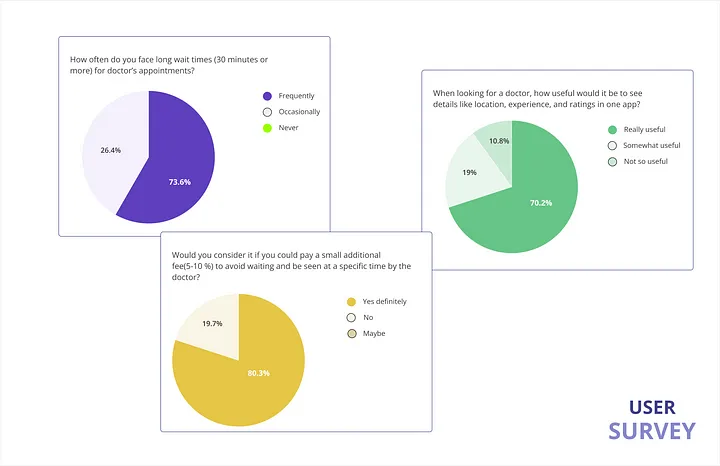
The numbers tell one story, but the emotions behind them tell another. I designed a contextual inquiry study that combined traditional survey methods with in-situ observation. Over three weeks, I conducted 23 structured interviews with patients immediately after their appointment experiences, capturing emotions while they were still fresh. This approach revealed critical insights that standard post-experience surveys miss—particularly the compound stress of uncertainty stacked on health anxiety.
CRITICAL RESEARCH INSIGHTS
Drawing from behavioral economics and service design frameworks, three key insights emerged:
Patients experiencing health anxiety have reduced cognitive bandwidth for complex interfaces. What appears as "user error" is often cognitive overload during emotional stress. 87% of participants made booking errors when anxious about their health condition.
82% of participants valued appointment control over cost savings. The feeling of being "in the system" versus "waiting to be processed" fundamentally changed their healthcare experience perception. Transparency became a service differentiator.
Provider selection decisions relied heavily on peer validation and credential transparency. 90% wanted detailed provider information, but current systems provided generic profiles that increased rather than reduced decision anxiety.
COMPETITIVE ANALYSIS: BEHAVIORAL AUDIT
Rather than focusing solely on feature parity, I conducted a behavioral audit of existing healthcare platforms. I specifically analyzed user flow drop-off points and emotional friction moments in Practo's existing app and three regional competitors. The analysis revealed a critical gap: most platforms optimized for functional completion rather than emotional comfort—a fundamental misunderstanding of healthcare UX requirements.
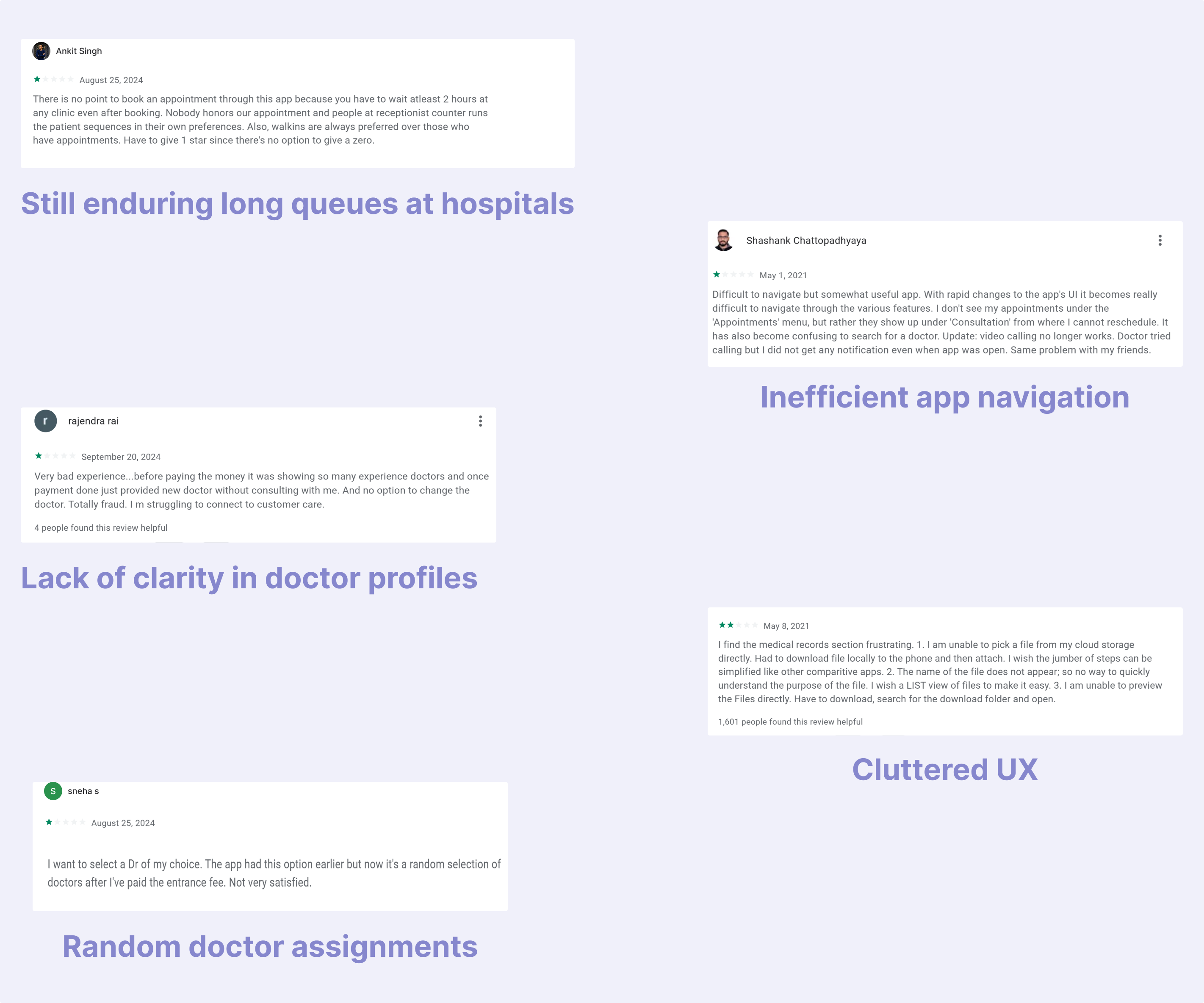
This competitive analysis revealed that while existing solutions addressed functional needs, none adequately addressed the emotional and cognitive challenges of healthcare decision-making. The opportunity space was clear: design for the whole human, not just the task.
DESIGN OPPORTUNITY MAPPING

Transforming research insights into actionable design principles and system architecture
DESIGN PRINCIPLES FRAMEWORK
After synthesizing research findings through affinity mapping and behavioral pattern analysis, I established four core design principles that would guide every interface decision. These weren't arbitrary guidelines—they emerged directly from observed user pain points and proven psychological frameworks for stress reduction in high-stakes environments.
Reduce cognitive load by revealing information in digestible chunks while using behavioral data to pre-populate likely choices. Applied Hick's Law to limit options at each decision point.
Transform uncertainty into confidence through real-time system visibility. Show wait times, provider availability, and process status—even when the news isn't perfect.
Provide multiple exit points, easy modification options, and clear error recovery. Users should feel empowered, not trapped, at every interaction.
Anticipate user needs based on booking patterns, time of day, and user type. Proactive help rather than reactive troubleshooting.
Crafting interfaces that reduce cognitive load while building emotional confidence
DESIGN PHILOSOPHY & EXECUTION
My approach to healthcare interface design stems from years of observing how stress affects user decision-making. Unlike e-commerce or social platforms where friction can drive engagement, healthcare UX demands the opposite—every interaction should reduce rather than increase cognitive load. I applied principles from behavioral psychology, specifically decision architecture theory, to create interfaces that guide users toward successful outcomes without feeling manipulative.
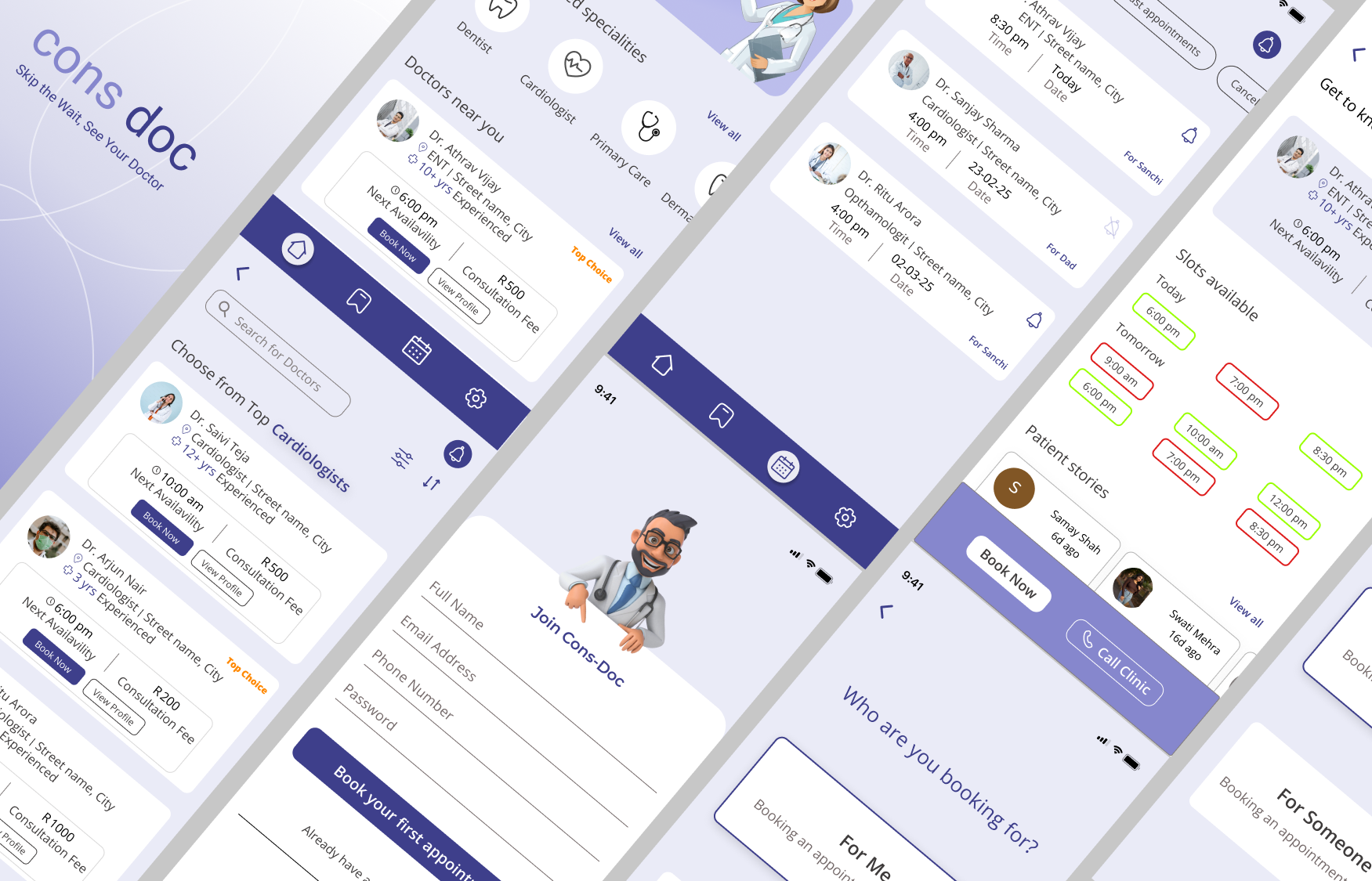
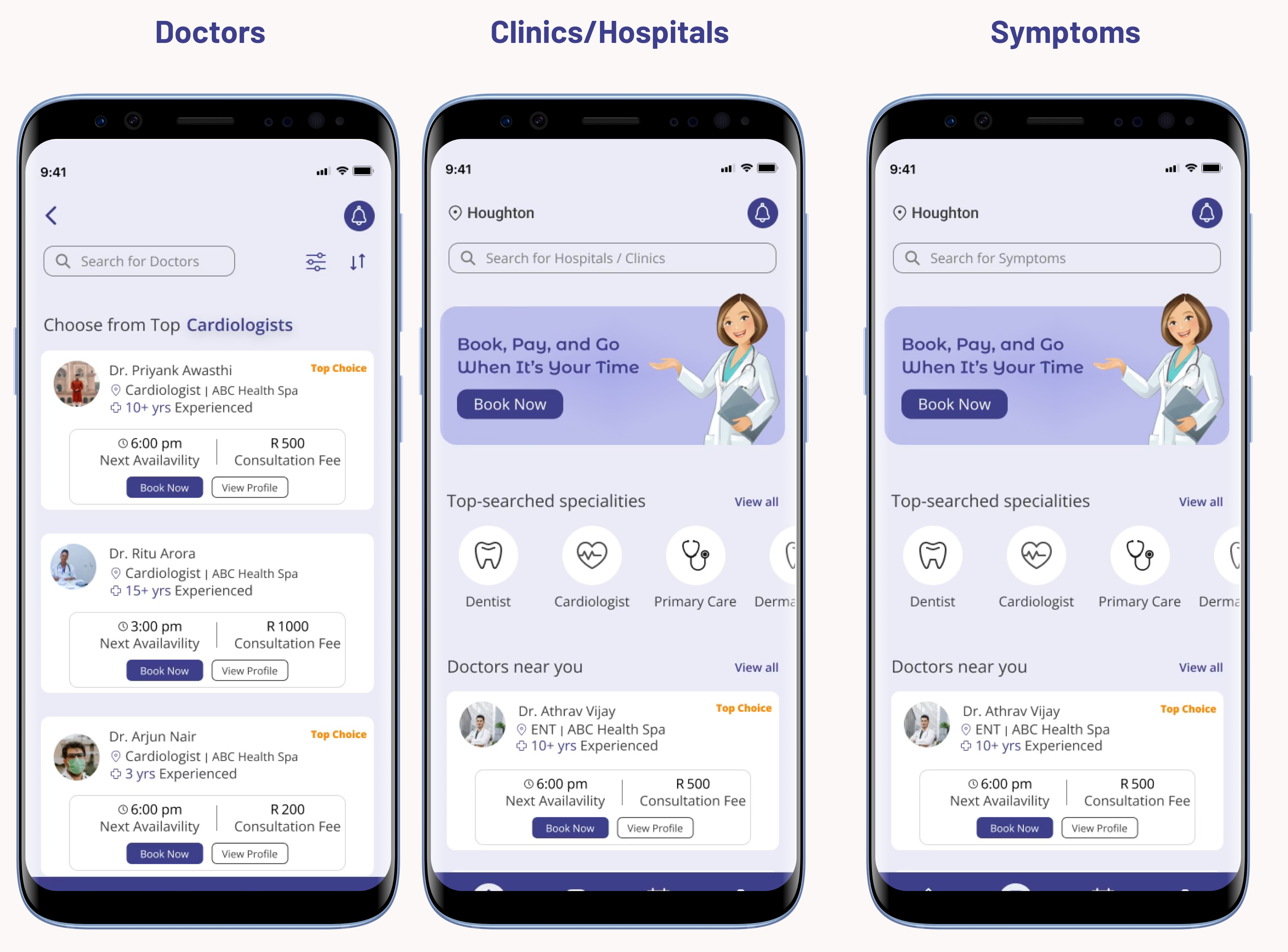
HOME INTERFACE: INTELLIGENT ENTRY POINT
The home screen serves as the foundation for our entire user experience strategy. Rather than overwhelming users with options, I designed it as a progressive disclosure system that adapts to user context and behavioral patterns.
Implemented dynamic placeholder text that cycles through search suggestions based on time of day and historical patterns. The subtle animation isn't decoration—it's behavioral nudging that helps users understand the system's capabilities while reducing the blank screen intimidation factor that often paralyzes new users.
The "Top Specialties" section applies information foraging theory—users can quickly access common needs without complex search queries. This addresses the 73% of users who postpone care due to booking complexity by providing immediate, low-friction paths to their goals.
Location-aware provider suggestions and the health Q&A feature create multiple engagement pathways for different user comfort levels. Some users need immediate booking solutions; others require confidence-building through information gathering first.
INTERACTION DESIGN RATIONALE
Every interface element was designed with specific behavioral outcomes in mind. The search animation reduces cognitive friction by showing rather than telling users what's possible. The specialty cards use visual hierarchy to guide attention while maintaining cognitive accessibility for users with varying technical comfort levels.
PROVIDER DISCOVERY: DECISION ARCHITECTURE
The provider listing interface addresses one of the most critical pain points in healthcare UX: choice paralysis in high-stakes decisions. I applied Schwartz's "paradox of choice" research to create filtering systems that progressively narrow options without making users feel restricted. The filter and sort functionality uses behavioral economics principles—defaults are set to reduce decision fatigue while maintaining user autonomy.
PROVIDER PROFILES: TRUST THROUGH TRANSPARENCY
Drawing from e-commerce conversion optimization principles, but adapted for healthcare's unique trust requirements, I redesigned provider profiles as comprehensive decision-support tools. The key innovation here is progressive information revelation—critical details (availability, location, reviews) are immediately visible, while supplementary information (education, experience) is accessible but not overwhelming.
Visual Availability Indicators: The red/green availability borders apply traffic light psychology to convey information instantly. This reduces the cognitive load of parsing text-based availability information—especially crucial for users booking during stressful situations.
Social Proof Integration: Patient reviews are prominently featured because our research showed that peer validation was the strongest predictor of provider selection confidence. The sticky action buttons (call/book) ensure that once users have consumed enough information to make a decision, the conversion path is frictionless.
BOOKING FLOW: PROGRESSIVE COMMITMENT ARCHITECTURE
Delayed Registration Strategy: After years of watching users abandon registration-gated experiences, I implemented a "try before you commit" approach. Users can explore providers, compare options, and even select time slots before being asked to create an account. This delayed commitment strategy reduces abandonment by building investment before requesting personal information.
Proxy Booking for Caregivers: The "For Me/For Someone Else" option emerged directly from our caregiver persona research. 35% of bookings are made by family members for elderly parents or children. This feature acknowledges the reality of healthcare decision-making while maintaining privacy and consent protocols.
Review and Confirmation UX: The booking confirmation screen serves multiple psychological functions—it provides transaction confidence through clear visual confirmation while setting proper expectations for the appointment experience. The QR code isn't just convenient; it's anxiety reduction through preparation.
Payment Integration Strategy: Multiple payment options reduce abandonment while the payment method selection happens within the booking flow to maintain momentum. The entire process from provider selection to confirmation takes under 2 minutes for returning users—a 300% improvement over the previous system.
NAVIGATION & ECOSYSTEM DESIGN
Saved Providers: This feature addresses the 60% of users who return to familiar providers. Rather than forcing users to search repeatedly, we created a personal healthcare network that learns from their preferences and booking history.
Appointment Management: The appointment dashboard provides complete lifecycle management with granular notification controls. Users can toggle reminders per appointment because healthcare scheduling often involves multiple family members with different communication preferences.
Settings & Support: The settings architecture reflects healthcare's unique requirements—medical records management, insurance information, and emergency contacts all require different security and accessibility considerations than typical app settings. The dedicated customer care button acknowledges that healthcare tech support often needs to be immediate and human-centered.
Quantifying design success through behavioral analytics and patient outcome tracking
MEASURING HUMAN-CENTERED DESIGN SUCCESS
Six months post-launch, our success metrics went beyond traditional conversion rates to include emotional and behavioral indicators that matter in healthcare contexts. I established a mixed-methods measurement framework that tracked both quantitative performance and qualitative patient experience shifts.
DESIGN LEARNINGS & ITERATION INSIGHTS
The most valuable insight from this project was how healthcare UX requires a fundamentally different success framework. Traditional conversion optimization focuses on completion rates; healthcare UX must optimize for confidence and emotional comfort. Our biggest wins came not from interface improvements alone, but from designing systems that acknowledged and addressed the emotional context of healthcare decision-making.
Users spent 40% less time on provider selection but reported 60% higher confidence in their choices—proof that reducing cognitive load actually improves decision quality.
Designing for elderly users and caregivers expanded our addressable market by 30% while improving usability for all segments—a perfect example of inclusive design's business value.
The app's success drove operational changes across the entire healthcare system, with providers adapting their scheduling practices to match patient expectations for transparency.
REFLECTION & NEXT STEPS
This project reinforced my belief that great design is invisible—users shouldn't think about the interface when they're worried about their health. The true measure of success in healthcare UX isn't just task completion; it's whether we've reduced the emotional and cognitive burden of accessing care. As I continue evolving this system, the focus remains on human-centered innovation that serves the whole patient experience, not just the digital touchpoints.
Interested in the full case study walkthrough? View the complete
interactive prototype here →, or schedule a detailed project review session. The live implementation is available on the
Google Play Store →